Abstract
Background: For research purposes, painful crises in sickle cell disease (SCD) have either been self-defined by patients, or adjudicated by research experts, most often based on whether urgent care or hospital care was sought for pain related to SCD. The Pain in Sickle Cell Epidemiology Study (PiSCES) determined that three-fourths of self-defined crises days were not managed in urgent or hospital care. The Analgesic, Anesthetic, and Addiction Clinical Trial Translations, Innovations, Opportunities, and Networks (AAPT) published a taxonomy of chronic SCD pain, defined as pain on most days of 6 months duration, along with at least one clinical sign, and no better explanation for the pain. We served on a similar SCD consensus panel to propose a more expansive taxonomy of acute sickle cell pain or painful episodes, informed by the PiSCES dataset (manuscript under review). Here we present three PiSCES-derived definitions of acute painful episodes, and we analyze the impact of various definitions on pain outcome results potentially useful for research.
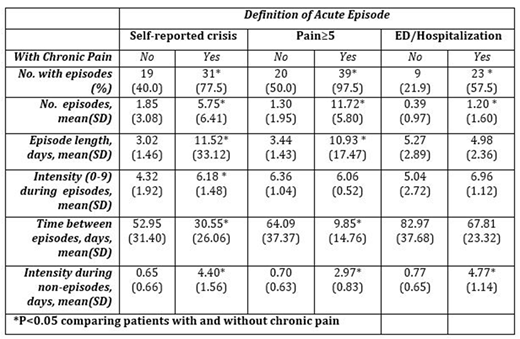
Methods: PiSCES Patients (N=81) who completed at least 5 out of the expected 6 months of daily diaries and did not have gaps in their daily diary of 4 days or more were included. Patients self-reported their worst sickle cell pain intensity on a scale from 0 (none) to 9 (unbearable), and independently self-reported whether they were having a crisis that day, whether they went for an unscheduled physician visit, an Emergency Department visit, or whether they were hospitalized for sickle cell pain. Definitions of acute pain episodes compared here include self-reported crisis days, days with pain ≥ 5, and days with utilization of the ED or overnight hospitalization (other potential definitions not shown). To meet any definition, a crisis day (pain≥ 5, utilization) had to be reported for 2 or more consecutive days. Non-crisis intervals were 2 or more consecutive days without a self-reported crisis (pain ≥ 5, utilization). The average length of non-crisis intervals was considered to represent the time between crisis episodes. For <4 consecutive missing days, imputations were performed using non-missing data to calculate the probability that missing days were crisis days. We used PiSCES data to compare various pain outcomes (see Table) for patients with and without AAAPT-defined chronic pain, for the three definitions of an acute painful episode. We note that episode length, intensity, time between episodes and intensity of non-episodes were all estimated using only patients who had an acute painful episode.
Results: (Table)
For each definition of an acute painful episode, a larger percentage of patients with chronic pain had acute episodes than patients without chronic pain. Similarly, chronic pain patients had statistically significantly more episodes and higher mean pain intensity on non-episode days. For 2 of 3 definitions (but not ED or hospitalization use), chronic pain patients had longer episodes and shorter time between episodes. Only for the self-reported crisis definition, patients had higher mean pain intensity during episodes. Raising the pain intensity threshold from 5 to 6 to define an acute episode slightly decreased the absolute percentage with acute episodes, the number of episodes, and the length of episodes, but did not affect the relationships between outcomes for patients with and without chronic pain (results not shown in table).
Conclusions: A comparison of various definitions of acute painful episodes using the PiSCES dataset yields slightly different pain outcome results. However, these differences are intuitive. For example, chronic pain patients still have more intense and more frequent acute painful episodes regardless of the definition used. The finding of more frequent acute pain in SCD adults with chronic pain has important implications for treatment and the design of SCD clinical trials.
Field:Ironwood: Consultancy, Research Funding; Prolong: Research Funding; Incyte: Research Funding. Dampier:Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal